Dementia Care During COVID-19
May 8, 2020
By Josef Halcomb
Dr Dylan Wint, Director of Clinical Operations at Cleveland Clinic, has explained that people with dementia are vulnerable to more severe complications due to COVID-19. In addition, abnormalities in the immune systems of individuals with dementia (most studied in Alzheimer’s disease but seen in other cases of dementia as well) and behavioral changes from dementia can increase risk of contracting the disease. For example, remembering to wash your hands regularly and not touch your face may be difficult for a person with dementia to begin doing every day.
While adjustments to mitigate the spread of COVID-19are necessary across all areas in long-term care (LTC) facilities, dementia care especially requires new modifications to lower the risk of infection for this more vulnerable population.
1. Promote Social Distancing
In order to practice safe social distancing, consider implementing the following adjustments to routine operations:
- Allow residents to eat in their rooms instead of in groups or a dining hall.
- Keep activities individualized.
- Adjust the building environment to keep residents safe, while allowing as much free will as possible. It is common for people with dementia to walk around and explore (sometimes called “wandering”) in a safe area, and this is an issue for facilities as they cannot restrain the resident and keep them in one place. Review the environment to see if there are ways you can allow residents to move around freely while incorporating safe social distancing.
2. Calm Family Members’ Concerns
Right now, family members are more nervous than ever. In most facilities, they are no longer able to visit their loved one and spend crucial time with them. For some with dementia, a familiar face or touch is core to curbing the degeneration caused by this disease. While its inevitably going to be a challenging time for families, here are a few ways you can help ease their concerns –
- Setting up family skype / video chats
- Contact the primary contact and arrange for a time you can help the resident with a video chat. Many free services, such as Zoom or Skype, are great options for staying connected to family and friends.
- Ensuring them the extra measures being taken
- Family members want to know what extra precautions are being taken in the air of COVID-19. Many LTC facilities have begun routine webinars to update family members extra steps they have enacted to make their facility a safer environment. Consider sending an email or a newsletter to keep families informed.
- Give them new ways to connect
- Allow family members to write emails and print it and read it to the resident. Likewise, if there is a white board or art supplies, have the patient draw or write a message to their family and then take a picture and email it to the family.
 Teepa Snow, an occupational therapist and dementia care educator, talks about other ways LTC facilities can help family members and dementia patients during this time here.
Teepa Snow, an occupational therapist and dementia care educator, talks about other ways LTC facilities can help family members and dementia patients during this time here.
3. Explaining COVID to dementia patients
Wearing gloves and masks may evoke questions as to “why”, or elicit reactions, from dementia residents who do not have an awareness of the pandemic or have forgotten. Residents with further-stage dementia may demonstrate behavioral reactions of frustration or confusion, especially if they struggle to effectively communicate or are non-verbal. As a caregiver, you must consider how you choose to respond.
Dr. Steven Sabat, neuropsychologist and Professor Emeritus of Psychology at Georgetown University, encourages caregivers to stick to the facts. Make sure you share what is going on calmly, without inducing any fear or panic. Choose words carefully that will mitigate anxiety, as well as simply explain why you are taking extra safety precautions during this time.
Here is an example of:
“Miss smith, there is a flu-like virus going around and we want to keep you and others as safe as possible. My mask and gloves are for your protection and mine”.
If despite providing a calm explanation, a resident appears uncomfortable receiving care due to the use of safety equipment (masks and gloves), get help or try again later. Follow your facility protocols to keep your residents safe while minimizing uncomfortable interactions with residents.
4. How to maintain hygiene (bathroom reminders, washing hands with them)
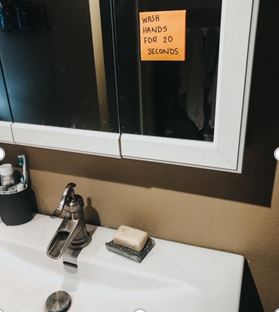
Encourage patients to wash their hands and avoid touching their face as much as you can. The Alzheimer’s Association recommends written reminders for support. Here are a few examples:
- A sticky note on the bathroom mirror reminding to wash hands for 20 seconds.
- A card to keep in their pocket that gives them a friendly reminder to practice good hygiene.
5. How to recognize symptoms
As dementia progresses, communication and expression can become a challenge. The individual may not be able to tell you how they are feeling or understand if they are feeling unusual with symptoms. For adults with dementia, you may first notice changes in their mood or behavior.
As a caregiver, be sure you take extra careful watch of these residents and monitor for symptoms which they may not verbally indicate to you. Here are the top symptoms of COVID-19, as outlined by the CDC:
- Cough
- Shortness of breath or difficulty breathing
Or at least two of these symptoms
- Fever
- Chills
- Repeated shaking with chills
- Muscle pain
- Headache
- Headache
- New loss of taste or smell
Be sure to monitor your residents for behavioral changes and physical symptoms of COVID-19. Consider taking their temperature daily or every few days, depending on the situation and requirements at your facility.
Simple Adjustments, Big Results
From these adjustments, you can reduce the spread of COVID-19 among adults with dementia and improve their wellbeing. Consider what you can do in your facility to make it a safer, better place during this pandemic.
For additional facts and clinical support to keep you informed during this turbulent time, click here to visit our COVID-19 resource portal.
Related Posts
More Tranquility Blogs
- Veterans and Incontinence
- Are Incontinence Pads the Right Product for Fecal Incontinence?
- How to Buy Adult Diapers: 4 Things to Consider
- 5 Tips for Discreetly Wearing Diapers in Public
- Why Double Diapering Is Not the Best Solution for You
- How to Choose the Best Bowel Incontinence Products and Diapers
- 5 Best Overnight Adult Diapers to Keep You Dry While You Sleep
- The Most Popular Types of Pads for Urinary Incontinence and Their Benefits
- 7 Tips for Finding the Best Diapers for Men
- 9 Tips for Finding the Best Women's Diapers to Stay Dry & Confident All Day




